Exploring the Complications of Psoriasis What You Need to Know
Are you living with psoriasis? or have a loved one who's been diagnosed? If so, you may have questions about the condition and complications of psoriasis. In this blog post, we'll explore the complications of psoriasis and what you need to know to address your concerns. We'll discuss the causes, symptoms, complications, and available treatments for psoriasis, as well as address how to manage flares and other health problems related to psoriasis. Read on to learn
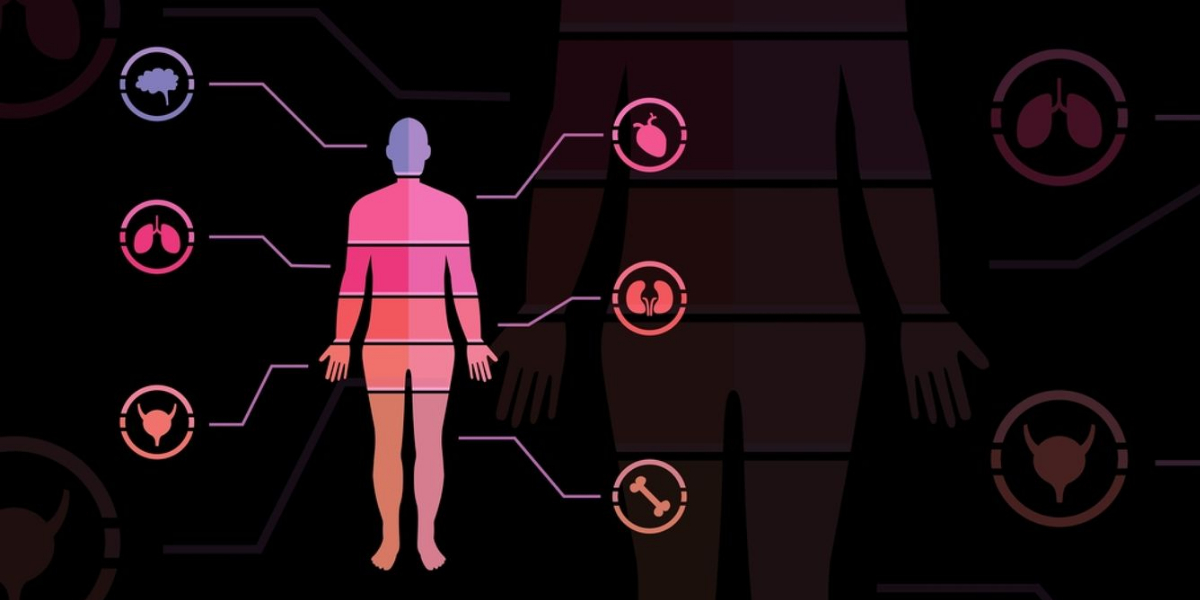
Psoriasis is a chronic auto-immune disease that affects the skin and can lead to many physical and emotional complications Not only can psoriasis cause red, inflamed patches on the skin, but it can also increase the risk of associated diseases such as heart attack, stroke, diabetes, and even depression. While there are treatments available to help alleviate some of these symptoms, it’s important to be aware of all the potential morbidities associated with this condition, Here are some of the potential complications of psoriasis:
Complications of psoriasis
Although a causal relationship has not been fully proven, there is evidence of various comorbidities due to psoriasis in many patients. Possible factors being considered as genetics, environmental factors, inflammatory pathways, and treatments exposed to the patient.
Anxiety and Depression
The first and possibly the most serious complication resulting from psoriasis is psychological distress due to the social stigma surrounding the disease. Many individuals may feel ashamed or embarrassed about their appearance and as a result, suffer severe anxiety and depression due to their perceived lack of control over their situation. It’s important for individuals suffering from psoriasis to seek out support if they find themselves feeling down or overwhelmed by their diagnosis.
Joint Damage or Psoriatic Arthritis
Psoriatic arthritis is an inflammatory joint disease that often occurs as a complication of psoriasis. This type of arthritis involves inflammation in both large and small joints and can result in pain, stiffness, and swelling. In some cases, it may require surgery or medications depending on the severity. Psoriatic arthritis can limit the movements of the joints and impacts the quality of life.
Metabolic syndrome
Metabolic syndrome is one with a high prevalence in patients with psoriasis. It is a complex of cardiovascular disease, insulin resistance, central adiposity, hypertension, abdominal obesity, and glucose intolerance which attributes the cardiovascular risk. 14 to 18 percent of psoriasis patients are estimated to have been affected with metabolic syndrome if the prevalence among the general population is taken as a baseline. Its high-frequency association in the psoriasis population is also independent of smoking and alcohol consumption. Also with the increase in the severity of the metabolic syndrome, there will be a progressive severity in psoriasis.
There are various diagnostic criteria developed for metabolic syndrome. However, widening waist circumference, spiking blood pressure, high triglycerides, HDL cholesterol levels, and higher fasting glucose levels are basic components looked out for metabolic syndrome before any further analyses.
Nonalcoholic steatohepatitis
Nonalcoholic steatohepatitis is a condition where fats infiltrate the liver usually in obesity. 47 percent of patients with chronic plaque psoriasis and only 26 percent of the non psoriatic population are affected by steatohepatitis. The affected liver produces interleukins and reactive proteins which cause an unwanted inflammatory burden, it also decreases the anti-inflammatory activity by decreasing the production of adiponectin. Infliximab, etanercept, PUVA, and phototherapy are considered treatments that have demonstrated significant results.
Insulin resistance and diabetes mellitus
Insulin resistance and diabetes mellitus are found predominantly in non-obese psoriasis patients. The threat of diabetes Mellitus is linear with the severity of insulin resistance. Infliximab exploits for treating these conditions and also for rheumatoid arthritis, spondylitis, Crohn’s disease, and obesity has proven to increase insulin sensitivity. In patients with lower plasma insulin, etanercept is suggested. For diabetes mellitus patients with altered glycemia, ustekinumab has demonstrated efficacy.
Obesity
Obesity is the root of metabolic syndrome and has a central role in all psoriasis comorbidities. Mainly seen in psoriatic arthritis patients, which worsens the complications of the existing disease and hinders the response to the treatment therapies. The use of infliximab, etanercept, ustekinumab, and adalimumab has even increased the mean weight gain in the patients and there is no decrease in BMI. Only the use of TNF agents did not induce any weight gain.
Cardiovascular disease
The auto-inflammatory response which goes on predominantly in psoriasis leads to insulin resistance as we saw above. This leads to diabetes mellitus and oxidative stress which ends up disturbing endothelial functioning. Thus the threat of atherosclerosis in the elderly or premature atherosclerosis at an early age arises. One reason for atherosclerosis put forth by research is the flow of psoriasis lesions into the blood which induces the appearance of vascular endothelial lesions. More than any healthy individual, the risk is for patients with psoriasis and psoriasis arthritis. Serious and major cardiovascular causes of myocardial infarction, heart stroke, and death are adverse occurrences.
Congestive heart failure
Moderate to severe psoriasis is said to increase the risk of heart failure. Methotrexate an inflammatory drug has an improvement in heart health and also the quality of life. TNF inhibitors although contraindicated are recommended after an echocardiogram. Ustekimub and apremilast are also safe to use.
Lupus and psoriasis
Both are autoimmune diseases but they are rare to coexist. But 1.1 percent of psoriasis patients have recorded lupus cases.
Eye Problems
Eye problems such as conjunctivitis and uveitis are rare complications found in psoriasis patients. One must regularly go through an eye examination when you are suffering from psoriasis to prevent eye damage.
Depression
Depression is of the common comorbidities. It is explained as a response to the psychological factors a patient goes through and impaired quality of life. Depression also leads to Alcohol abuse, obesity, etc
Kidney Diseases
Kidney problems are another potential morbidity linked to those suffering from psoriasis due to inflammation caused by their immune systems attacking healthy cells in their body including organs like kidneys which could lead to kidney failure or infection over time. Additionally, certain medications used to treat psoriatic conditions might put additional stress on your renal system leading to further complications later down the line if caution isn’t taken beforehand when looking into treatment options.
Skin infections
People with psoriasis are more prone to developing skin infections, as the damaged skin barrier makes it easier for bacteria to penetrate the skin. Common infections include impetigo, cellulitis, and staph infections.
Conclusion
In conclusion, Psoriasis is a serious skin condition that carries many complications and risks. While it is best managed through regular medical interventions and treatments, understanding the potential risk factors and morbidities associated with psoriasis can help you maintain better overall health. With a good understanding of the available treatments, lifestyle modifications, and self-care advice for those living with psoriasis can increase the quality of life.
References:
- González-Parra E, Daudén E, Carrascosa JM, Olveira A, Botella R, Bonanad C, Rivera R; en representación del Grupo de Trabajo en Inflamación Sistémica en Psoriasis. Kidney Disease and Psoriasis. A New Comorbidity? Actas Dermosifiliogr. 2016 Dec;107(10):823-829. English, Spanish. doi: 10.1016/j.ad.2016.05.009. Epub 2016 Aug 3. PMID: 27497509.
- Constantin MM, Ciurduc MD, Bucur S, Olteanu R, Ionescu RA, Constantin T, Furtunescu F. Psoriasis beyond the skin: Ophthalmological changes (Review). Exp Ther Med. 2021 Sep;22(3):981. doi: 10.3892/etm.2021.10413. Epub 2021 Jul 12. PMID: 34345263; PMCID: PMC8311223.
- Teng Y, Xie W, Tao X, Liu N, Yu Y, Huang Y, Xu D, Fan Y. Infection-provoked psoriasis: Induced or aggravated (Review). Exp Ther Med. 2021 Jun;21(6):567. doi: 10.3892/etm.2021.9999. Epub 2021 Mar 29. PMID: 33850539; PMCID: PMC8027725.
- https://pubmed.ncbi.nlm.nih.gov/30017705/
- https://pubmed.ncbi.nlm.nih.gov/34122426/
- https://pubmed.ncbi.nlm.nih.gov/30509759/