Erythrodermic Psoriasis Treatment
Psoriasis is a skin disease known to be the most prevalent autoimmune disease among humans. The precise etiology of psoriasis is poorly understood but it is a result of a complex interaction between the skin, genetics, immune system dysfunction, environment, and triggers.
Psoriasis is characterized by sharply demarcated erythematous plaques covered with silver scales. The regions most affected are the scalp, the trunk, the extensive surfaces, and the lumbosacral region. The other clinical symptoms of psoriasis include itch, pain, and scales. Several variants of psoriasis are inverse, guttate, pustular, and erythrodermic psoriasis etc.
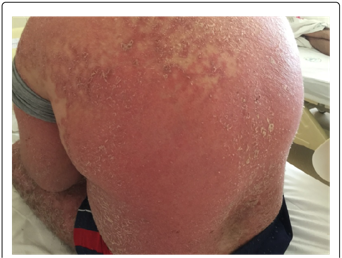
Erythrodermic psoriasis is a severe and rare form of psoriasis that affects the entire body. It is characterized by widespread redness, inflammation, and scaling of the skin. Erythrodermic psoriasis can be a life-threatening condition and requires immediate medical attention.
Erythrodermic psoriasis is a rare variant of psoriasis with an estimated prevalence of 1 to 2.25 percent among psoriatic patients. Prior retrospective studies have shown it is more common in elderly men of 53 years and above than in women. In recent data, the cases of erythrodermic psoriasis have become even lower.
Symptoms of erythrodermic psoriasis
The symptoms of erythrodermic psoriasis include severe redness and inflammation of the skin, which may be accompanied by itching, pain, and a burning sensation. The skin may also appear scaly and may shed in large sheets. Other symptoms can include fever, rapid pulse, changes in body temperature, and fluid and protein loss leading to edema (swelling).
- It typically presents with changes in the skin. Erythema which is the redness of the skin is the characteristic symptom of erythrodermic psoriasis. Pruritus, scales, hair loss, desquamation, and psoriatic plaques are the others.
- The erythema involves more than 75 to 90 percent of the body’s surface area.
- The clinical symptoms include mild leukocytosis, elevated serum C reactive protein, liver dysfunction, elevated serum creatinine, hyperkeratosis, regular acanthosis, lymphocyte infiltration, dilated blood vessels, agranulocytosis, etc., consistently with the symptoms of psoriasis.
The triggers of erythrodermic psoriasis
- Erythrodermic psoriasis can be triggered by various factors, including sudden withdrawal of systemic psoriasis treatment, severe sunburn, infection, certain medications (such as corticosteroids), and other types of psoriasis that are poorly controlled.
- Emotional stress, exposure to intense ultraviolet exposure, addiction to alcohol, HIV infection, use of tar products, and abrupt withdrawal of oral or topical corticosteroids and methotrexate therapies, certain therapies and drugs cause psoriasis, cancers and underlying chronic diseases, etc will trigger flares of erythrodermic psoriasis.
Complications of erythrodermic psoriasis
- Severe and fatal complications like acute kidney failures, sepsis, respiratory distress, electrolyte imbalance, severe anemia, protein depletion, altered thermoregulation, and cardiac failure.
- Erythrodermic psoriasis is also one of the first manifestations of HIV.
- Erythrodermic psoriasis can lead to serious complications, such as dehydration, infection, pneumonia, and congestive heart failure. The disrupted skin barrier can also make the body more susceptible to bacterial, viral, and fungal infections.
Diagnosis of erythrodermic Psoriasis
- Psoriasis is a multifactorial disease. It occurs in different forms and includes extracutaneous signs of disease.
- The disease type is classified based on the severity, age of occurrence, morphology of the skin, and physical symptoms.
- Diagnosis is usually made based on a physical examination and medical history. A skin biopsy may be performed to confirm the diagnosis and rule out other conditions.
- After a thorough assessment of the physical manifestations, the dermatologist will run further tests assessing the clinical symptoms.
Erythrodermic Psoriasis Treatment
- Erythrodermic psoriasis treatment is typically aggressive and aimed at stabilizing the condition and relieving symptoms. It often requires hospitalization. Treatment may include topical therapies, oral medications, phototherapy, and systemic treatments such as biologics. Supportive care, including fluid replacement, temperature regulation, and infection prevention, is also crucial.
- Treating erythrodermic psoriasis involves treating neutrophilia, eosinophilia, and leukocytosis, regulating elevated serum C reactive protein and elevated creatinine, hypoproteinemia, liver dysfunction, hypocalcemia, etc.
- The course of treatment is planned to clear the scale and erythema first and psoriasis next. Triamcinolone 0.1% is prescribed as an ointment for two weeks under occlusion. Ixekizumab is added for psoriasis dosing.
- Oral prednisone and ixekizumab, cyclosporine, antihistamine, cetuximab, apremilast, topical corticosteroids, topical vitamin D3 analogues, and ultraviolet B (UVB) therapy are the treatment options for erythrodermic psoriasis.
- Antiretroviral therapy, Thai herbal therapy, and Chinese ( tripterygium wilfordii) and Western herbal medicines (chamomile, St.John’s’s Wort) as topical herbal treatments are useful in the treatment of psoriasis.
- Ayurvedic psoriasis treatment is found beneficial in managing psoriasis and preventing its reoccurrence.
It’s important for individuals with erythrodermic psoriasis to work closely with a dermatologist or healthcare provider experienced in treating severe psoriasis. The condition requires prompt medical attention and ongoing management to minimize complications and improve quality of life.
Reference: