Nail psoriasis symptoms and treatment
Nail psoriasis is a chronic condition that affects the nails, typically due to psoriasis, a skin disorder characterized by red, scaly patches. Nail psoriasis can cause a variety of changes in the nails, including pitting, discoloration, thickening, crumbling, ridges, and separation from the nail bed.
Nail psoriasis is seen in 80 percent of psoriasis patients with psoriatic lesions. This is common in patients with skin disease, especially during psoriasis arthritis. Nail psoriasis is extensively more common in the elderly.
80 to 90 percent of psoriasis patients with psoriatic lesions are involved with the nails. However, 80 percent of them are associated with psoriatic arthritis, and only a fraction of them about 5 percent are involved with isolated nail psoriasis. 90 percent of the patients living with cutaneous psoriasis also have nail psoriasis. 87.5 percent of the patients living with psoriatic arthritis have nail psoriasis.
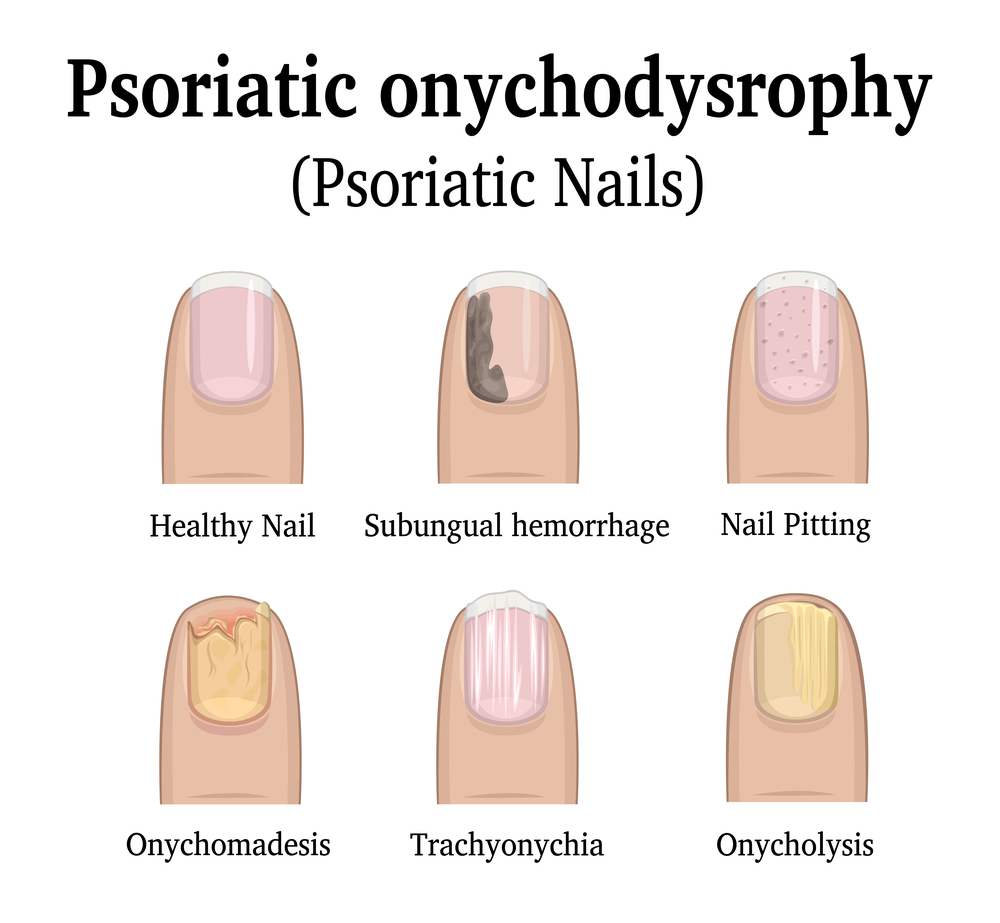
Nail psoriasis images


Symptoms of nail psoriasis
The symptoms of nail psoriasis vary from person to person but commonly include nail pitting (small depressions or dents in the nails), yellowish discoloration, thickening of the nails, crumbling or flaking, ridges or grooves, and separation of the nail from the nail bed (onycholysis). The condition can cause discomfort, pain, and functional impairment.
- In the elderly population, it is challenging to diagnose nail psoriasis precisely because of the nail changes that happen with aging.
- Napolitan nail pattern is seen in the elderly where the nail colour changes from pale pink to yellow, grey, and white.
- A Neapolitan ring pattern, with the absence of a lunula. And white and pink ridges appear on the nails.
- Thinning of fingernails, thickening of toenails, the slower nail growth rate.
- Flattening of fingernails, transverse growth of the fingernails, horizontal peeling of layers, and brittleness in the nails
- Nail pitting is the most common symptom of the nail; psoriasis is seen in 68 percent of patients.
- When affected with psoriasis, the nail matrix shows nail pitting, leukonychia, and red spots in the lunula.
- Nail bed psoriasis shows onycholysis, oil spots that appear as pink spots under the nails due to the trapping of serum and debris, splinter hemorrhages, and nail bed hyperkeratosis
- Leukonychia, which is white nails, is observed under the nails.
- Nail dystrophy is predominant in nail psoriasis with all these changes in colour, texture growth, and shape.
- Sphincter hemorrhages which mean the red blood spots lying longitudinal under the nails, which bleed initially
- Onycholysis is seen in 67.2 percent of patients in which the nail appears to be separated from the nail bed.
- Subungual hyperkeratosis is seen in which the skin cells accumulate excessively in between the nail and nail bed
- Aging nail changes in the elderly also interfere with the symptoms of nail psoriasis.
Nail psoriasis causes
Nail psoriasis is thought to be an autoimmune condition, where the immune system mistakenly attacks healthy cells in the body. Genetic factors and certain triggers, such as trauma to the nails, infections, or stress, can contribute to the development or worsening of nail psoriasis.
The exact mechanism behind nail psoriasis is not fully understood, but it is believed to be related to an immune system dysfunction and genetic factors. Here’s a general overview of the mechanisms involved in nail psoriasis:
- Immune system dysfunction: Nail psoriasis is considered an autoimmune disorder, where the immune system mistakenly attacks healthy cells in the body, including the skin and nails. In psoriasis, immune cells called T cells become overactive and trigger inflammation in the skin and nail tissues.
- Genetic factors: There is a strong genetic component to psoriasis, including nail psoriasis. Certain genes have been identified that are associated with an increased risk of developing psoriasis. However, having these genes does not guarantee that a person will develop the condition.
- Hyperproliferation of skin cells: In individuals with nail psoriasis, there is an abnormal acceleration of the growth cycle of skin cells. Normally, skin cells go through a cycle of growth and shedding over the course of a few weeks. In psoriasis, this process is significantly accelerated, leading to an accumulation of skin cells on the surface of the skin and nails.
- Inflammatory response: The immune system response triggers an inflammatory reaction in the affected nail tissues. This inflammation leads to the characteristic symptoms of nail psoriasis, such as pitting, discoloration, thickening, and separation of the nail from the nail bed.
- Disruption of nail matrix: The nail matrix is the area at the base of the nail where new nail cells are produced. In nail psoriasis, the inflammation and abnormal skin cell growth can disrupt the nail matrix, leading to the development of nail abnormalities, such as pitting and ridges.
It’s important to note that the exact mechanisms underlying nail psoriasis may vary among individuals, and more research is needed to fully understand the condition. Additionally, environmental factors, such as trauma to the nails, infections, or stress, can also contribute to the development or worsening of nail psoriasis in susceptible individuals.

Nail psoriasis treatment
Treating nail psoriasis can be challenging, as the nails grow slowly and topical treatments may not penetrate deeply enough to reach the affected areas. Treatment options for nail psoriasis include topical corticosteroids, calcipotriol or calcitriol (vitamin D analogues), topical retinoids, intralesional corticosteroid injections, systemic medications (such as methotrexate, cyclosporine, or biologics), and phototherapy. Nail care practices like keeping the nails trimmed, moisturized, and protected can also help manage symptoms.
- The severity of the nail psoriasis is assessed by certain scales called psoriasis severity assessment index and nail assessment and psoriatic arthritis and nail psoriasis quality of life
- The penetrability of the topical medications depends on the site of inflammation. Therefore a clearer diagnosis of nail bed and nail matrix psoriasis is necessary.
- Topical super potent steroids and vitamin D analogues clobetasol propionate and calcipotriol the first line treatment also with intralesional steroid injections, for mild psoriasis.
- Second-line treatment includes topical steroids, topical vitamin D analogues, combinations of topical D analogues with topical steroids, topical retinoids, and topical keratolytic agents such as urea nail lacquer, salicylic acid, or topical 0.1% tacrolimus ointment.
- Topical corticosteroids are another most frequently used medication in the form of emulsions, creams, ointments, and nail lacquers. Steroids are combined with systemic therapy for more benefits.
- Combination therapy with vitamin D analogues. These vitamin D analogues regulate proliferation, and cell differentiation and are anti-inflammatory.
- Tazoretene has great efficacy as a topical treatment for nail psoriasis. It is tolerable with limited side effects reported.
- Topical cyclosporine and tacrolimus are the topical calcineurin inhibitors that are prescribed to inhibit gene action. This treatment is relatively highly tolerable and the side effects are very little.
If you suspect you have nail psoriasis, it is recommended to consult a dermatologist for an accurate diagnosis and appropriate treatment plan. They will evaluate your symptoms, perform a physical examination, and may order additional tests, such as nail clippings or biopsies, to confirm the diagnosis and rule out other conditions.
It’s important to note that the information provided here is not a substitute for medical advice. If you’re experiencing symptoms of nail psoriasis or have concerns about your health, please consult a healthcare professional for proper evaluation and guidance.
Reference:
- Abdullah L, Abbas O. Common nail changes and disorders in older people: Diagnosis and management. Can Fam Physician. 2011 Feb;57(2):173-81. PMID: 21321168; PMCID: PMC3038811.
- https://www.sciencedirect.com/science/article/abs/pii/S0733863520301145
- https://pubmed.ncbi.nlm.nih.gov/34478047/
- https://pubmed.ncbi.nlm.nih.gov/35697407/
- https://www.sciencedirect.com/science/article/abs/pii/S0733863520301170
- https://doi.org/10.1016/j.det.2020.12.011
- https://doi.org/10.1016/j.ad.2022.01.006
